A CASE OF 60 YR OLD FEMALE
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's consent.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs in the comment box below.
Note : This is an ongoing case and will be updated regularly.
Date of admission: 01/12/2023
Chief complaint :
A 60 Yr old female, unemployed, resident of chinnakapati (nalgonda district) was brought to the casualty with c/o prolonged abnormal involuntary movements bilaterally in both upper and lower limbs for duration of > 30 minutes.
History of Presenting Illness:
Patient was apparently asymptomatic 23 years ago when she had first episode of fits (after sustaining a head injury due to fall 7 years before her first episode) .Each episode begins with patient feeling dizzy, uprolling of eyes, headache radiating from front to back of right side of head only(does not radiate to other side); dragging type of pain, deviation of mouth, clasping of hands, tongue bite followed by loss of consciousness ->falls to the floor -> each episode lasts for 10 to 15 minutes.
Post episode: After returning back to consciousness she complains of headache, post ictal confusion and not able to recollect any event during episode.
Patient is on phenytoin 100mg (Eptoin) for the same since 23 years.
She also took ayurvedic medications for same (Medication not specified)
Frequency of attack: 0- 2 /year
Precipitating factorsfor each attack include mental stress reagrding family and sleeplessness.
Current episode:
On 01/ 12/ 2023, patient felt uneasy and had headache and was on empty stomach.
When attempted to lie down eventually developed fits which continued for > 15 minutes for close about 30 minutes .
She presented similarly as in presented in previous attacks for which she was rushed to the emergency department after prolonged abnormal involuntary movements for > 30 minutes.
Past history:
•Patient was admitted in hospital 2 times before for similar complaints ( but each episode lasting for only 15 minutes)
•No history of DM/ HTN/ Asthma/ CKD/ TB/Thyroid disorders
•H/o 3 cesarean sections; no h/o of any other surgeries.
Family history:
No similar complaints in the family
Personal history:
•Diet: Mixed
•Appetite: Normal
•Sleep: Adequate
•Bowel and bladder movements: burning micturition +, Bowel movements are normal
•Addictions: -
•Allergies: avoids brinjal, gongura
General Examination
Examination was performed after taking consent.
•Patient is conscious, coherent, cooperative
•Moderately built
•Moderately nourished
•No pallor, icterus, cyanosis, clubbing, koilonychia, pedal edema, lymphadenopathy
Right eye
Vitals:
At the time of admission:
•BP: 110/60 mmhg
•PR: 133 bpm
•Temperature: 102°F
•GBRS: 222 mg/dl
•SPO2: 88%@RA
When recorded later
•BP: 140/80 mmhg
•PR: 128bpm
•RR: 24cpm
•Temperature: febrile to touch
• SPO2: 94%@RA
Systemic Examination:
CNS:
•Level of consciousness: stuporous
•Speech: No response
•Attitude and position: Patient was lying on the bed in supine position
•Bulk of muscles
•Cranial Examination: could not be elicited
•Sensory Examination: could not be elicited
•Motor Examination:
Tone: Normal in both upper and lower limbs
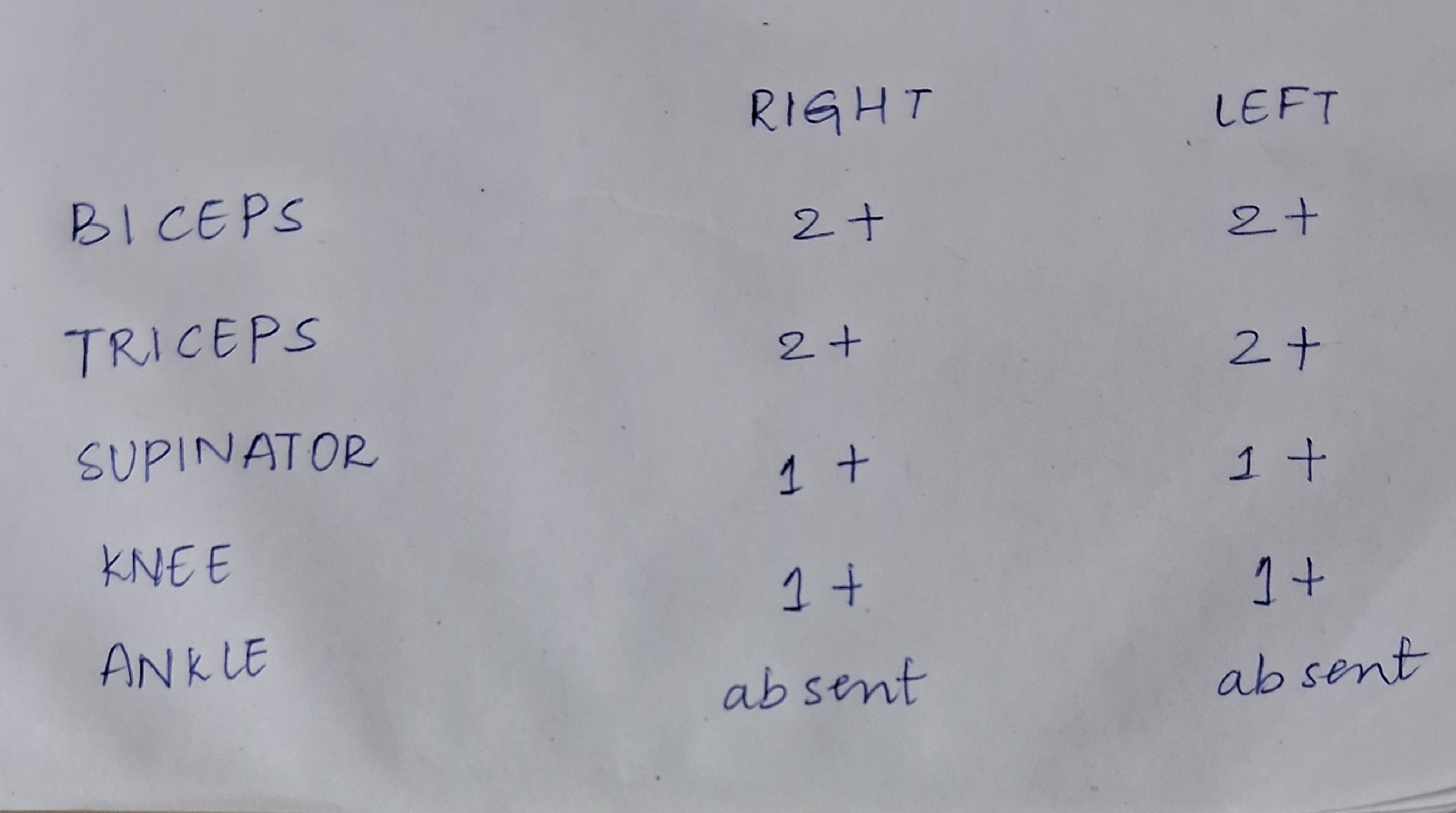
Reflexes:
Superficial Reflexes:
1) Corneal- present
2) Conjunctival- present
Deep tendon Reflexes:
•Gait: could not be elicited
•Cerebellar signs: could not be elicited
CVS:
Inspection:
•Chest bilaterally symmetrical
•No precordial bulges found
•Trachea appears to be central
•No scars or sinuses seen
•JVP not seen
•Bilateral air entry +
Palpation:
•Apical impulse is felt
Auscultation:
•S1,S2 heard
•No murmurs heard
Respiratory system:
Inspection:
•Chest bilaterally symmetrical
•No precordial bulges found
•Trachea appears to be central
•No scars or sinuses seen
•No visible pulsations
•Bilateral air entry +
Palpation:
•Trachea is central in Position ( assessed by 3 finger method)
•All inspectory findings were confirmed
•No local rise of temperature
•No tenderness elicited
Percussion:
•Resonant note heard in all quadrants
Auscultation:
•Normal vesicular breath sounds +
Per abdomen:
Inspection:
•Shape of abdomen: non distended
•No scars and sinuses seen
•No visible pulsations
•No visible peristalsis observed
Palpation:
•All inspectory findings were confirmed
•On Palpation, abdomen is soft, non-tender
•No organomegaly
•No local rise of temperature
Percussion:
•Resonant note in all 9 regions
Auscultation:
•Bowel sounds +
Provisional Diagnosis:
Generalised tonic clonic seizures secondary to acute CVA
INVESTIGATIONS : 01/12/2023
ULTRASOUND
MRI
BLOOD GLUCOSE LEVEL
RANDOM BLOOD GLUCOSE
POST PRANDIAL BLOOD GLUCOSE
HbA1C
SERUM - MAGNESIUM
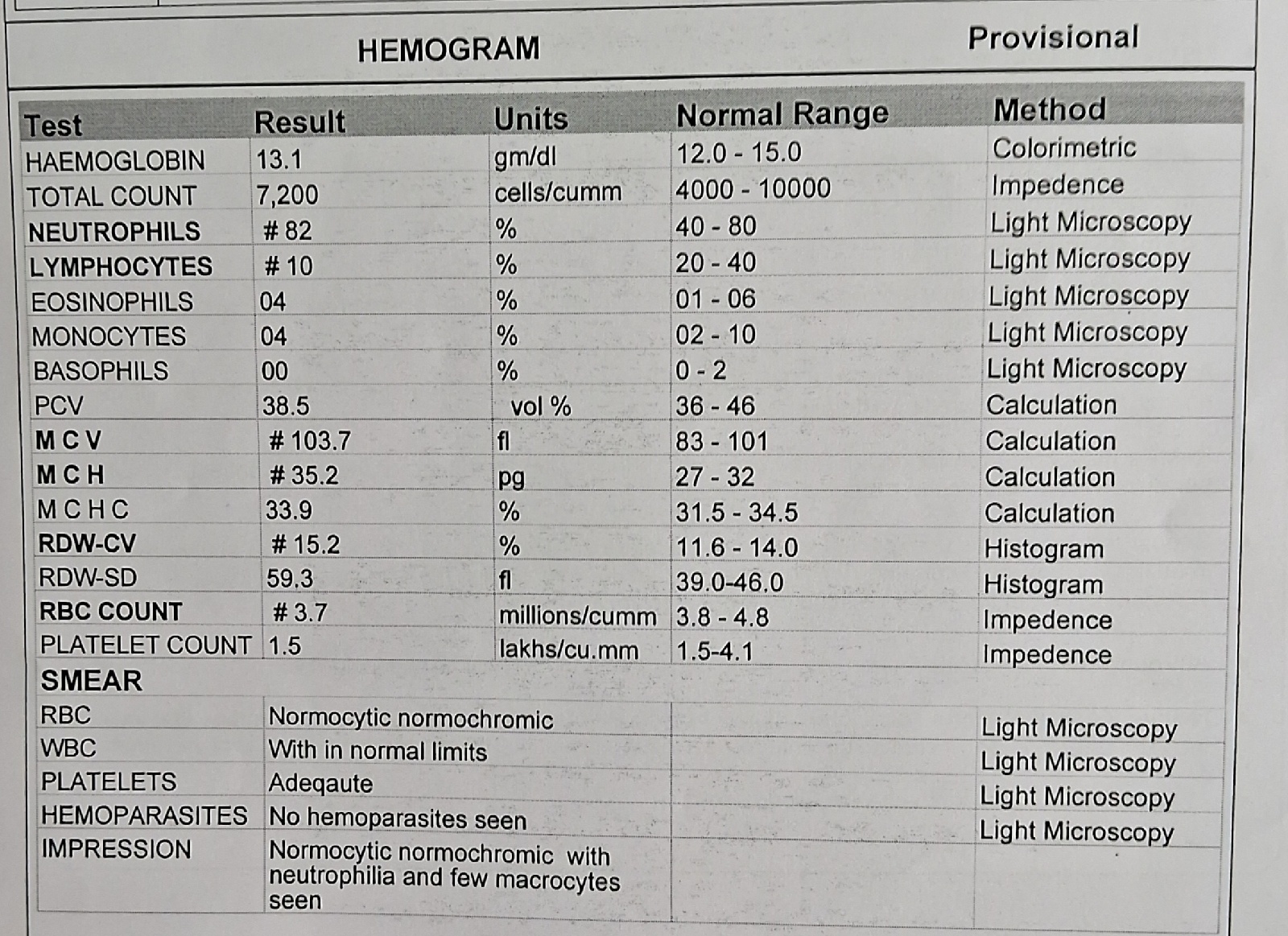
COMPLETE BLOOD PICTURE
BT AND CT
Treatment :
a)IV FLUIDS 10NS
b) inj.loraz 2cc iv Stat
c)inj levipil 2gm iv Stat
d) TAB. Atorvastatin 40mg PO/ Stat
e)TAB ecospirin 325mg PO
f) TAB. Ceftriazone 2mg iv BID
g) inj.optineuron 1 amp in 500ml NS
h)TAB. Clopitab 350mg /PO/ STAT
02/12/2023
VITALS:
•BP: 120/ 70 mmhg
•PR: 85 bpm
•RR: 22cpm
•Temperature: 97.8°F
•GBRS:117 mg/dl
•SPO2: 94@ RA
Systemic Examination:
CNS:
•Level of consciousness: stuporous
•Speech: No response
•Attitude and position: Patient was lying on the bed in supine position
•No signs of meningitis
•Cranial Examination: could not be elicited
•Sensory Examination: could not be elicited
•Motor Examination:
Tone: Normal in both upper and lower limbs
Power: Absent in both upper and lower limbs
Reflexes:
Superficial Reflexes:
1) Corneal- present
2) Conjunctival- present
•Gait: could not be elicited
•Cerebellar signs: could not be elicited
CVS:
Inspection:
•Chest bilaterally symmetrical
•No precordial bulges found
•Trachea appears to be central
•No scars or sinuses seen
•JVP not seen
•Bilateral air entry +
Palpation:
•Apical impulse is felt
Auscultation:
•S1,S2 heard
•No murmurs heard
Respiratory system:
Inspection:
•Chest bilaterally symmetrical
•No precordial bulges found
•Trachea appears to be central
•No scars or sinuses seen
•No visible pulsations
•Bilateral air entry +
Palpation:
•Trachea is central in Position ( assessed by 3 finger method)
•All inspectory findings were confirmed
•No local rise of temperature
•No tenderness elicited
Percussion:
•Resonant note heard in all quadrants
Auscultation:
•Normal vesicular breath sounds +
Per abdomen:
Inspection:
•Shape of abdomen: non distended
•No scars and sinuses seen
•No visible pulsations
•No visible peristalsis observed
Palpation:
•All inspectory findings were confirmed
•On Palpation, abdomen is soft, non-tender
•No organomegaly
•No local rise of temperature
Percussion:
•Resonant note in all 9 regions
Auscultation:
•Bowel sounds +
INVESTIGATIONS:
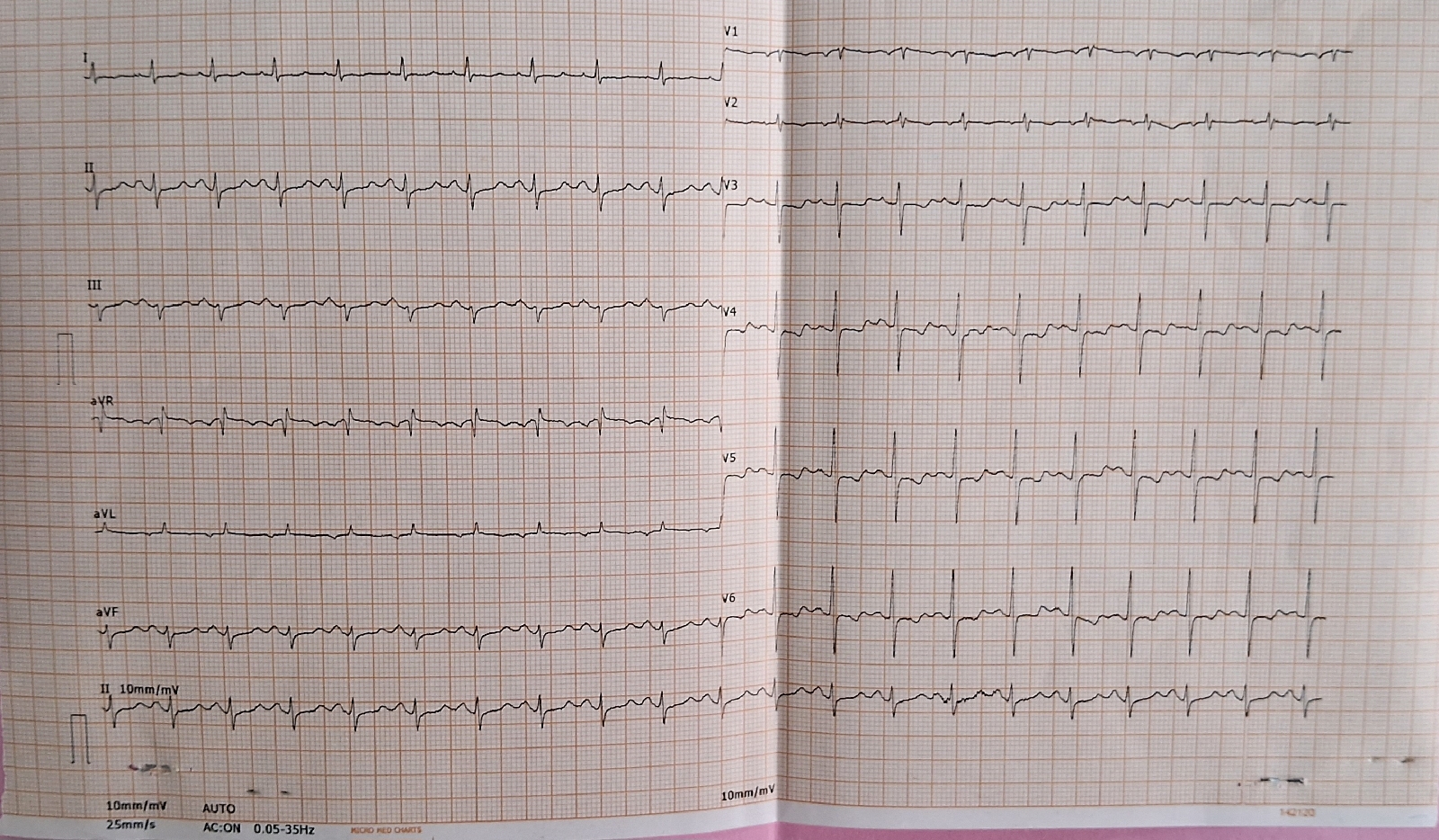
ELECTROCARDIOGRAM
FASTING BLOOD GLUCOSE LEVEL
COMPLETE BLOOD PICTURE
PROTHROMBIN TIME
APTT( COAGULATION PROFILE)
Treatment :
a)IV FLUIDS 10NS @75 ml/hr
b) inj.loraz 2cc iv
c)inj levipil 1gm iv/BD
d) TAB. Atorvastatin 40mg PO OD
e)TAB ecospirin 75mg/ PO OD
f) TAB. Ceftriazone 2mg iv BID
g) inj.optineuron 1 amp in 500ml NS
h)Monitor Vitals 4th hourly
g)check seizure activity
03/12/2023
VITALS
•Pulse rate: 86 bpm, regular rhythm, Normal volume and character , character of vessel wall is good.Radio radial delay could not be assessed due swelling in left hand
•Blood pressure: 100/ 60 mmhg; taken in right arm in sitting Position
•Respiratory rate: 23 cpm, thoracoabdominal type
•Temperature: Afebrile to touch
INVESTIGATIONS
ECHOCARDIOGRAM
VITALS :
REFLEXES :
BICEPS REFLEX
KNEE REFLEX
FEVER CHART


























Comments
Post a Comment